News
-

UPHS – Bell Heroes | Jill Dix
February 20, 2026What is your role at UPHS – Bell?I am a registered nurse case manager at UPHS – Bell.What was your inspiration for getting into healthcare?I knew I wanted to work in a field that had many different options and opportunities. When I was a kid, I didn’t always know what I wanted to do when I grew up, but when I found that nursing and healthcare had a wide…
Learn more -

UP Health System – Portage Honors Matthew Williams with the Sunflower Award
February 13, 2026UP Health System – Portage is proud to recognize Matthew Williams, elder associate, as this quarter's recipient of the Sunflower Award. The Sunflower Award recognizes outstanding employees at UP Health System – Portage who demonstrate excellence through teamwork, a positive attitude, strong communication and deep knowledge in their roles. These…
Learn more -

UPHS – Marquette Heroes | Lisa Gauthier
February 13, 2026What is your role at UPHS – Marquette? I am the Patient Safety Report (PSR) Supervisor at UP Health System – Marquette. What was your inspiration for getting into healthcare? What inspired me to work in healthcare is the opportunity to help people feel better—inside and out.
Learn more -

UP Health System – Marquette offers new procedure for atrial fibrillation
February 12, 2026UP Health System – Marquette (UPHS – Marquette) is now offering pulsed field ablation (PFA), a minimally invasive outpatient procedure to treat atrial fibrillation (AFib), the most common type of abnormal heart rhythm.
Learn more -

UP Health System – Portage Honors Hannah Ruohonen, RN, and Kayla Williamson, RN, with the DAISY Award
February 11, 2026UP Health System – Portage is proud to recognize Hannah Ruohonen, RN, and Kayla Williamson, RN, as this quarter’s recipient of the DAISY Award for Extraordinary Nurses®. The DAISY Award is part of the DAISY Foundation’s mission to honor the exceptional, compassionate care nurses provide to patients and families every day.As a nurses in the…
Learn more -

Women and heart health: The conversation we need to be having
February 11, 2026When people think about the biggest health risks facing women, heart disease often does not top the list. Cancer, breast health or reproductive concerns are usually the first things that come to mind. The reality, however, is clear: Cardiovascular disease is the leading cause of death among women in the United States. Despite this, fewer than half of women recognize heart disease as their greatest health threat. That lack of awareness matters because heart disease does not develop overnight. It progresses quietly over time, often beginning much earlier in life than most women realize.
Learn more -

UPHS – Portage Heroes | Kara Galbraith
February 06, 2026What is your role at UPHS – Portage?I'm an administrative secretary and patient advocate.What was your inspiration for getting into healthcare?After many years working in elementary schools, I felt it was time for a challenge – one that would allow me to help people in a more direct way and make a meaningful, positive difference in their lives. That desire led…
Learn more -

UPHS – Marquette Heroes | Stacy Kohl, BSN RN
February 06, 2026What is your role at UPHS – Marquette? I am a clinical manager in the Intensive Care Unit (ICU) and the Intermediate Care Unit (IMCU) at UP Health System – Marquette. What was your inspiration for getting into healthcare? Since I was a child, I have wanted to be in healthcare. My inspiration to be a nurse is my mother. She became an LPN when I was a teenager. Her drive and dedication to her schooling while working and taking care of her family showed me it was possible.
Learn more -

UPHS – Bell Heroes | Tara Alderton
January 30, 2026What is your role at UPHS – Bell?I am a certified medical assistant in occupational medicine at UP Health System – Bell.What was your inspiration for getting into healthcare?Helping people has always been a passion of mine. I strive to be someone patients are comfortable coming to when they are in need.What’s a typical day like for you? What is it like…
Learn more -

Imaging Services that Specialize in You
January 30, 2026At UP Health System – Portage, we provide quality imaging services with advanced technology, including Nuclear Medicine and Positron Emission Tomography (PET). Our nuclear medicine camera does a variety of tests and scans to help diagnose a medical issue and to start you on your road to recovery — offering fast 3D imaging and better sensitivity.Nuclear…
Learn more -

UPHS – Marquette Heroes | Leanna Taylor, RN
January 30, 2026What is your role at UPHS – Marquette? I am a registered nurse in the neonatal ICU at UP Health System – Marquette. What was your inspiration for getting into healthcare? When I was in high school, I really enjoyed anatomy and physiology classes and thought I wanted to become a doctor. My senior year, I had an internship on the cardiac unit here and was really drawn to the care and compassion of bedside nursing.
Learn more -

UP Health System – Bell Honors Makenzie Laakso, RN, with the DAISY Award
January 23, 2026UP Health System – Bell is proud to recognize Makenzie Laakso, RN, Emergency Department, as this quarter’s recipient of the DAISY Award for Extraordinary Nurses®. The DAISY Award is part of the DAISY Foundation’s mission to honor the exceptional, compassionate care nurses provide to patients and families every day.As a nurse in the Emergency…
Learn more -
UP Health System – Portage Heroes | Joan Kotila
January 23, 2026What is your role at UP Health System?I am a phlebotomist at UP Health System – Portage. I perform outpatient and inpatient blood draws, as well as community draws. I also conduct DOT drug screenings and breath alcohol testing.What’s a typical day like for you? What is it like working in this field?I got into healthcare because I lost my mom at a young age and…
Learn more -
UPHS – Marquette Heroes | Wendi L. Tonkin
January 23, 2026What is your role at UPHS – Marquette? I am a patient service representative supervisor at UP Health System – Marquette. What was your inspiration for getting into healthcare? I have always had a strong interest in the medical field. Healthcare is both challenging and rewarding, and I enjoy the opportunity to learn new things.
Learn more -

UP Health System – Marquette names Teresa Perry chief financial officer
January 22, 2026MARQUETTE, Mich. — Jan. 22, 2026 — UP Health System – Marquette announced today that Teresa Perry, MBA, CPPS, has been named chief financial officer.Perry brings more than 17 years of experience within UP Health System to the role. Most recently, she served as chief financial officer at UP Health System – Bell, a position she held for the past 12…
Learn more -
.jpg)
Healthy Habits to Start in 2026 for Better Overall Health
January 19, 2026The start of a new year is often a time for people to take a closer look at their health and the habits that shape it. While many people set ambitious resolutions, steady, realistic adjustments are more likely to lead to lasting results At UP Health System in Michigan's Upper Peninsula, primary care providers…
Learn more -

UPHS – Bell Heroes | Samantha Dymond
January 16, 2026What is your role at UPHS – Bell?I'm a clinic nursing supervisor at UP Health System – Bell. What was your inspiration for getting into healthcare?Healthcare felt like a natural fit. The goal was always to help someone in need. And now, I get to support a strong clinical team during the process.What’s a typical day like for you? What is it like…
Learn more -

UPHS – Marquette Heroes | Lindsay Williams
January 15, 2026What is your role at UPHS – Marquette? I am a medical assistant for Digestive and Liver at UP Health System – Marquette. What was your inspiration for getting into healthcare? I've always had the desire to help people. I now have the honor of being one of the first faces people see when they come into the clinic. Whether it's setting people up for procedures or providing emotional support in times of need, I am fulfilling that longing to help others.
Learn more -
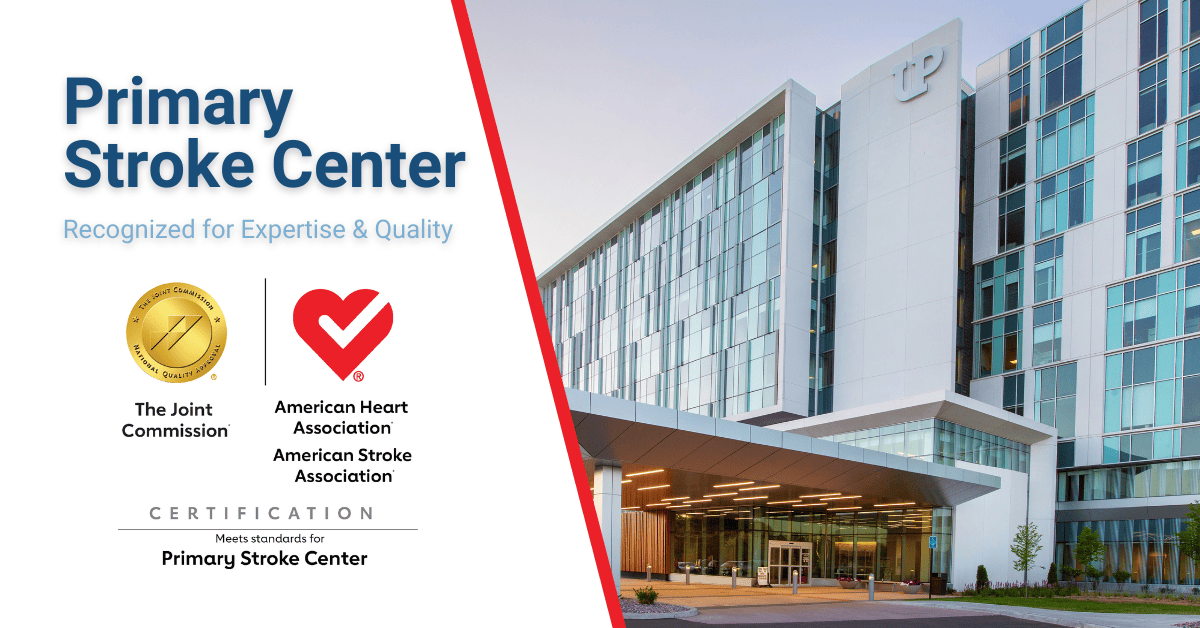
UP Health System – Marquette Awarded Primary Stroke Center Certification from Joint Commission
January 13, 2026MARQUETTE, Mich. (Jan. 13, 2026) — UP Health System – Marquette (UPHS – Marquette) has earned Joint Commission’s Gold Seal of Approval® and the American Stroke Association’s Heart-Check mark for Primary Stroke Center Certification. UPHS – Marquette underwent a rigorous, onsite review on October 23, 2025, as part of the process…
Learn more -
UP Health System – Portage Heroes | Renée Laitila
January 09, 2026The main lobby information desk at UP Health System – Portage plays a vital role in creating a smooth, welcoming experience for every patient and visitor who enters the facility. Positioned just inside the main entrance, the information desk serves as the first point of contact, helping patients navigate updated appointment processes and directing them efficiently…
Learn more
